May 18, 2016
InnomarLive Recap A Comprehensive Look at Rare Disease in Canada
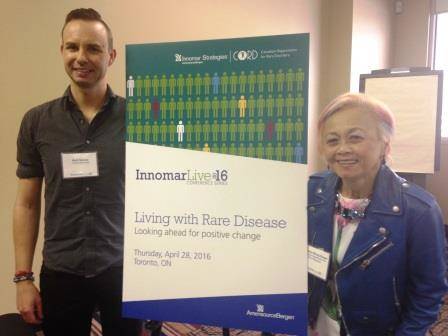
Picture: Matthew George, Rare Disease Patient Advocate (Left);
Durhane Wong-Rieger, President & CEO, CORD (Right)
“Living with Rare Disease: Looking Ahead for Positive Change” was an interactive meeting featuring a diverse panel of speakers, including:
- Durhane Wong-Rieger, President and CEO of Canadian Organization of Rare Disorders (Chair)
- Dr. Robert Hegele, Department of Medicine, London Health Sciences Centre
- Don Husereau, Institute of Health Economics
- Matt George, Patient Advocate
- Cathy Parker, Health Canada
- Dr. Chander Sehgal, Canadian Agency for Drugs and Technologies in Health
- Stephen Frank, Canadian Life and Health Insurance Association Inc.
- Sandra Anderson, Innomar Strategies
Participants in the afternoon session had a unique opportunity to gain valuable feedback on their strategic questions, through one-on-one sessions with the speakers.
Key Takeaways
The panelists covered many diverse stakeholder perspectives within rare disease. Key takeaways from the meeting included:
- Health Canada continues to move forward with its Orphan Drug Framework.
- Adaptive Pathways and Managed Access Programs (MAPs) could increase timely access to drugs for rare diseases in Canada.
- Generation of real-world evidence is required to support a Managed Access model.
- Patient advocacy is critical to shaping policy, gaining access to effective treatments and supporting patients and their families with rare diseases.
Regulatory Considerations for Rare Disease
From a regulatory perspective, Canada is one of the few developed-world jurisdictions without a framework for the authorization of orphan drugs. Approximately 60% of US orphan drugs have received market authorization in Canada.1 Continued access after the conclusion of trials and funding by the provinces are common concerns.
Health Canada is developing an Orphan Drug Framework for Canadians. The framework objectives include channeling orphan drugs into a federal regulatory pathway designed to improve market availability in Canada, and aligning, where possible, with other international regulators’ orphan drug frameworks and the funding recommendation process. The Orphan Drug Framework will seek public input into the review of submissions for orphan drugs.
The Adaptive Pathway model may provide timely access to new medicines in rare disease by balancing medical need with information on the benefits and risks of orphan drug medications. The concept proposed for drugs for rare diseases (DRDs) in Canada is that of “coverage with evidence development” which could involve: early approval of orphan drugs based on life-threatening or severely debilitating conditions with no other effective treatments, regulatory approval of orphan drugs requiring ongoing data collection, and patient registries to collect post-market safety and effectiveness information.
For orphan drugs facing a highly challenging reimbursement environment, Managed Access Programs (MAPs) and Adaptive Listing models may provide potential solutions that will require generation of evidence.
Patient Support Programs in Rare Disease
A Patient Support Program in rare disease provides an opportunity to leverage data to support real-world evidence generation to address the needs of payers. Considerations for the development of orphan program solutions include:
- implementation of a central registry/Patient Support Program model;
- genetic testing requirements; and
- data collection criteria based on approved guidelines.
Payer Participation
Public payers can support a rare disease strategy by providing sustainable access to promising therapies (e.g. consider offering a unique model based on outcomes for rare diseases). Private payers can provide timely, equitable and evidence-informed care. Manufacturers can generate real-world evidence to meet market access needs (e.g. through disease burden studies to demonstrate unmet clinical needs and support advocacy initiatives for rare diseases).
Collaboration between Public and Private Payers
Private payers expect the number of expensive orphan drugs on the Canadian market to increase, leading to a growing fiscal impact from ultra-rare treatments on insurers. Both government and private payers face the challenges of providing access to DRDs while creating a financially sustainable system.
For example, collaboration between the public and private sectors could involve:
- joint public/private assessment of the available clinical evidence
- joint development of common criteria for access to each new orphan drug
- joint pricing negotiation
- ongoing collection of real world evidence and reporting to a central location for review
- transparent judicial process for removing non-responders from therapy
Patient Advocacy
Advocacy is critical for patients’ access to effective treatments for rare disorders, and provides much-needed support to individuals and their families who are struggling with potentially devastating diseases.
In the words of the Canadian Organization of Rare Disorders, “We believe that now is the time to act to provide hope and treatment to Canadians and their families who are impacted by a rare disease.”
REFERENCES
1. Canadian Organization of Rare Disorders website. Available from: https://www.raredisorders.ca/our-work/
